Role of care team

The changing SMA landscape
After patients are treated, health professionals who care for patients with SMA have a role to play. Learn from SMA experts about ongoing care and the future of SMA after treatment.
Transcript
Transcript: EXPERTZ – ONGOING CARE AND THE FUTURE OF SMA
ZOLGENSMA (onasemnogene abeparvovec-xioi) is a gene therapy for the treatment of pediatric patients less than 2 years of age with spinal muscular atrophy (SMA).
ZOLGENSMA has a Boxed Warning for Serious Liver Injury and Acute Liver Failure. Please see additional Important Safety Information at the end of this video. Please see the accompanying Full Prescribing Information.
EXPERTZ: Medical Experts Series
DR TESI ROCHA
We see that the field is evolving, the phenotype is evolving so because of that education is key.
DR SHIEH
We’re really still working out the details of these emerging phenotypes.
DR RAO
A 360-degree approach is absolutely essential. You need to have partners. You need to leverage expertise in different fields.
What type of providers are on an SMA care team?
DR SHIEH
It’s important to realize that SMA treatment is individualized. Every patient has different needs. Some patients, for instance, need more pulmonary care. Some patients need more physical therapy. Perhaps some patients also need more orthopedic interventions.
DR RAO
When we receive the newborn screen results, there’s a large team that goes into action, and this team is a multidisciplinary team that is involved in taking care of the child. The initial members who receive the diagnosis are the neurologists and the genetic counselors. They have the patient scheduled with the neurologist to go over the diagnosis and the treatment options. But along with that, we make sure that the rest of our team is ready to take care of the patient clinically. And the team does involve members from the physical therapy sciences, occupational therapy, our dietician, our pulmonologist, all of them are aware of a new diagnosis and are ready to see the child if needed.
TESI ROCHA
We also have pulmonologists, cardiologists, orthopedic doctors, and bone health specialists—endocrinologists—that are part of that team. In certain circumstances, we also have a palliative care team as well. And I like to emphasize that palliative care team shouldn’t be end of life decision making. They’re a great group actually at the time of the diagnosis. And many times, we work with them, particularly when there are ethical questions that come up, and we respect those coming from the families so that is a team that we also work quite closely with.
How has SMA changed with treatment?
DR TESI ROCHA
We are now facing a different type of disease than the one that we used to face before the treatment.
DR RAO
I am really fortunate to see this in evolution, in my own practice and in my own training. I have seen SMA Type 1 children who were never destined to even live, let alone sit or stand or walk—doing that. So disease modifying agents have really revolutionized the natural history of progression for SMA. So the question then arises in our mind if they were not supposed to sit, stand, or walk, how are their bodies now going to handle this?
DR SHIEH
One of the interesting observations we’ve made is that there are emerging phenotypes in patients with SMA now that they’re undergoing treatment. For instance, we have patients who are now perhaps able to sit but are developing significant scoliosis at a very young age. So the truth is, emerging phenotypes have never been dealt with before. We don’t really have a consensus on how to treat these types of problems.
DR TESI ROCHA
But it’s very exciting times for us to be able to have these problems, these new problems regarding SMA care. But we have to keep our eyes wide open, not only for the modifications in the phenotype, but also the potential side effects and long-term effect of the medications. So we always prioritize safety.
DR RAO
So seeing these patients over time, following them up, making sure we have a close observation is very, very important to not only study the new natural history of SMA but to intervene proactively with what we see is coming that we wouldn’t have expected before the disease-modifying treatments were so successful.
What should other HCPs know about SMA?
DR RAO
When I trained in this field, we were handful of people around the country trying to do this. So the whole field has taken hundred steps forward because there are treatment options, not just for families, but for teams and for the future generations who want to train in this and do this, both as their career and as their calling.
DR SHIEH
What I want to make sure everyone realizes is that SMA is now a treatable disease. Patients are now, with treatment, living longer lives with a better quality of life as well. And so what we’re going to see is a transformation of patients with SMA.
DR TESI ROCHA
These are great, these are fascinating times for someone with SMA, and for all the medical community to have options in terms of treatment. But I think that this is just the beginning. And so, we need time to follow the patients down the road and see what to expect of the long-term effects of these medications.
DR RAO
I think one has to always make sure that the families are front and center through all of this. And whatever steps we take for even better treatments in the future should always be centered around the family unit.
VOICE-OVER
Please see additional Important Safety Information at the end of this video.
Monitor patients at baseline and for at least 3 months following ZOLGENSMA infusion.
Please Full Prescribing Information for complete pre- and post-treatment requirements.
The impact of immediate referral and treatment
If you suspect or recognize the signs of SMA, it is essential you refer your patient to a relevant specialist who can promptly diagnose and treat SMA. Early action helps prevent permanent motor neuron loss. Due to the progressive nature of SMA, patients who are treated earlier often see better outcomes.3
Pediatric healthcare professionals, physical therapists, pulmonologists, and genetic counselors are among those who may encounter an undiagnosed patient with SMA in their practice.4,5
Suspicion of SMA should trigger immediate action. Flag your referral for urgent consultation.
Unsure where to go?
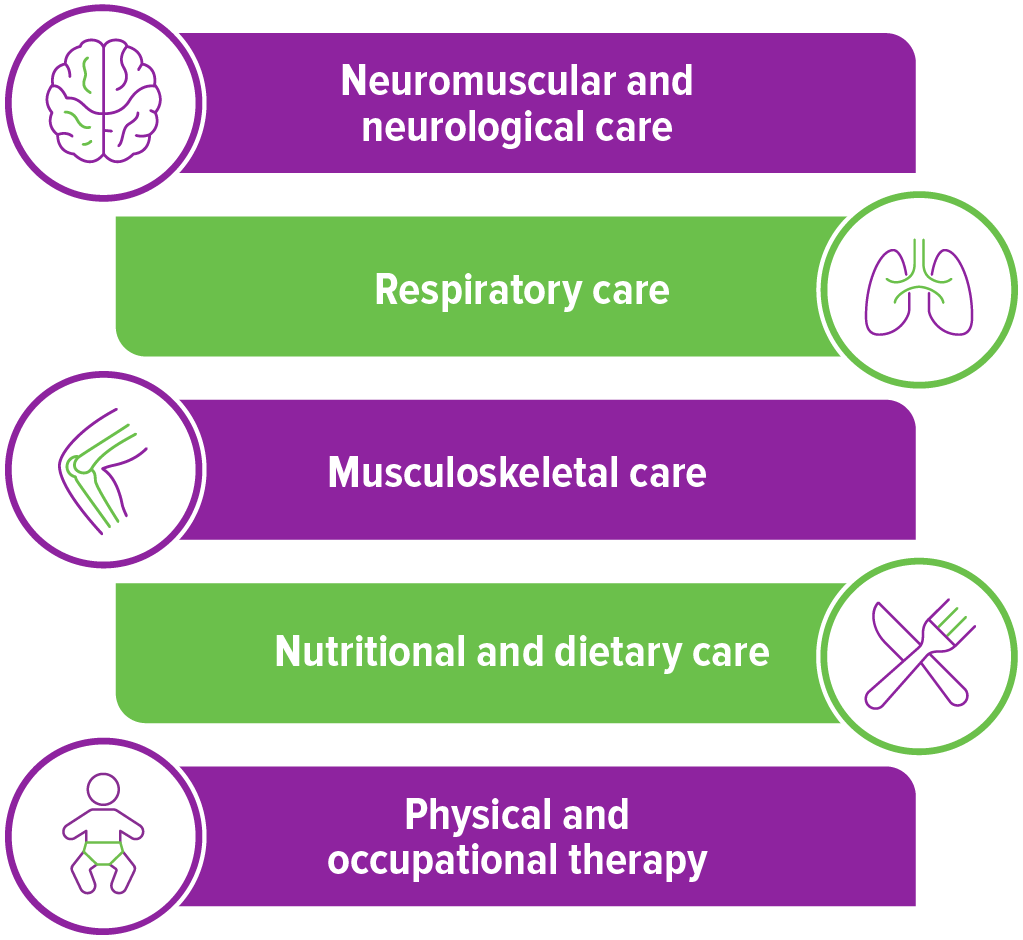
Ongoing care requires a multidisciplinary care team
Even after disease-modifying treatment, patients with SMA may need respiratory, nutritional, and musculoskeletal support. The team will vary from patient to patient, but a coordinated team of specialists can help monitor the patient’s SMA.4,5
It is recommended that a neurological expert, such as a pediatric neurologist or neuromuscular specialist, coordinate the care of the patient, as they will likely have the most experience with anticipating needs.4
While the specific needs and support levels of patients differ, part of the ongoing care can include an assessment of motor function, which may include regular sessions with a physical therapist and possible use of braces. Additionally, nutritionists can be involved to monitor weight and nutrient intake, paying careful attention to calcium and vitamin D for bone health.4
References: 1. Lin CW, Kalb SJ, Yeh WS. Delay in diagnosis of spinal muscular atrophy: a systematic literature review. Pediatr Neurol. 2015;53(4):293-300. 2. Schorling DC, Pechmann A, Kirschner J. Advances in treatment of spinal muscular atrophy—new phenotypes, new challenges, new implications for care. J Neuromuscul Dis. 2020;7(1):1-13. 3. Glascock J, Sampson J, Haidet-Phillips A, et al. Treatment algorithm for infants diagnosed with spinal muscular atrophy through newborn screening. J Neuromuscul Dis. 2018;5(2):145-158. 4. Mercuri E, Finkel RS, Muntoni F, et al. Diagnosis and management of spinal muscular atrophy: part 1: recommendations for diagnosis, rehabilitation, orthopedic and nutritional care. Neuromuscul Disord. 2018;28(2):103-115. 5. Wang CH, Finkel RS, Bertini ES, et al; Participants of the International Conference on SMA Standard of Care. Consensus statement for standard of care in spinal muscular atrophy. J Child Neurol. 2007;22(8):1027-1049.